New guidance published to support women transitioning from fertility to maternity care
RCN’s Professional Lead for Midwifery and Women’s Health Carmel Bagness blogs about the ‘Transition from Fertility to Maternity Care’ guidance that aims to support both patients and healthcare professionals.
Becoming pregnant is emotional, being both joyous and filled with anxiety.
In September 2022, the Royal College of Nursing (RCN) published new guidance on Transitions from Fertility to Maternity Care, which can be found here. This guidance came about as a result of concerns expressed about how the journey between a positive pregnancy test, following fertility treatment, and the safe birth of a baby, can be complex when moving from fertility to maternity services, and more importantly overwhelming with challenges for women and their partners.
The project to develop these guidelines set about understanding the patient journey and providing information about the possible pathways of care for women and others (their partners/support networks) as they travel through their fertility treatment and pregnancy, and how they can best be supported by the health care professionals they encounter along their journey.
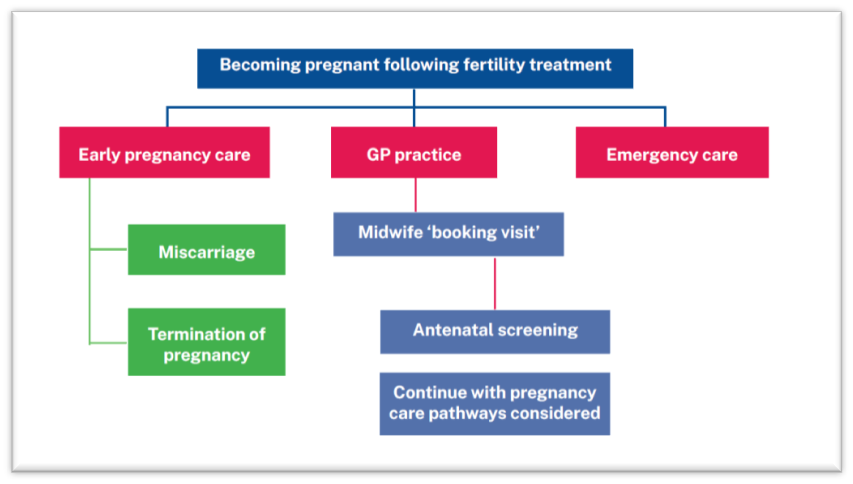
The project team included healthcare professionals and those representing patient groups, which provided rich discussion and some clear messages, about information giving, joining up services and understanding the particular journey that an individual, their partner/network and family has been on. The RCN guidance provides an overview of what care is available, and is outlined in the table below.
Commissioning of NHS services varies across the four nations and is often commissioned to the private sector. The majority of care does takes place in the independent sector and is self-funded.
Once a pregnancy is confirmed, women are usually discharged from the fertility service, and many describe a feeling of being cast adrift, and not knowing where to access care. Until a pregnancy is confirmed it can be too challenging to even think of the next steps if treatment is successful so they know little if anything about local maternity services. Becoming pregnant is emotional, being both joyous and filled with anxiety.
Ideally, once discharged from fertility care, the women can book an appointment to see their midwife, however there can be a gap in this process of some weeks, and women (and their partners/support networks) are often left anxious and unsure about how to proceed.
RCN recommends that all those discharged from fertility services with a positive pregnancy outcome must be given written information about local Early Pregnancy Care (EPC) services, maternity services and emergency care services, should they require help, reassurance or support until they meet the midwife who will care for them though their pregnancy.
Many are not aware of the early pregnancy care that is available through most local NHS Trusts, and may resort to continuing to have private ultrasound scans to provide some reassurance about their progress until such time as they have contact with a midwife. The Association of Early Pregnancy units (AEPU), identifies over 200 EPC units across the UK, which are listed on their website.
Those seeking fertility care do so for a variety of reasons, both medical and non-medical, and the make up a family unit varies enormously, therefore it is important for healthcare professionals to better understand the needs of all those who become pregnant, their partners/networks, intended parents and family. This includes those from LGBTQIA+ (lesbian, gay, bisexual, transgender, queer/questioning (one’s sexual or gender identity), intersex, and asexual/aromantic/agender)) communities, who will have different needs in all three areas of care, and this is explored throughout the guidance.
Another area for consideration is to better understand the journey of those who identify as coming from ethnic and minority groups including Gypsy, Roma and traveller communities, whose needs and experience may also differ.
Joined up services are a key element of successful care and the need for service level agreements between the services, and an understanding of each other’s roles across the three key services of fertility care, early pregnancy care and maternity services, is seen as critically important to improving the care provided.
Although many pregnant women receive excellent care, and understanding from the services they encounter, it is imperative that fertility nurses understand the onward journey, whilst midwives also need to better understand the history of those who have been though fertility care to achieve a pregnancy. It is always important to ask the woman about her journey so far. Overall a greater understanding of the gap in services and the potential for patients to feel anxious and unsure of where to seek help, requires greater understanding of early pregnancy care services in the local area. It is hoped that the RCN guidance will provide information and ideas on how this can be better achieved.

Carme Bagness, Professional Lead Midwifery and Women’s Health, Royal College of Nursing.
Carmel is a midwife and nurse, with almost 40 years’ experience in healthcare. She is currently working as the professional lead at the Royal College of Nursing. She has previously worked in midwifery practice, leadership, higher education and at the Department of Health. Her professional interests are in women’s health and wellbeing, midwifery and fertility care. This includes looking at how education and awareness can be enhanced in areas such as menstrual wellbeing and menopause. She has also focused on care improvements for those who may be more vulnerable, such as those impacted on by female genital mutilation, domestic abuse and modern slavey.
Twitter: @CarmelBagness; Facebook: Carmel Bagness.
Review date: 15 April 2027

